
What are the aims of this leaflet?
This leaflet has been written to help you understand more about topical corticosteroids. It tells you what they are, how they work, how they are used, and where you can find out more about them.
What are topical corticosteroids and how do they work?
Steroids are naturally occurring hormones, produced in the body. There are different types of steroids. A synthetic (man-made) steroid is commonly used to treat skin problems. It is called a corticosteroid. Corticosteroids treat skin conditions by reducing inflammation (red and itchy) and make the skin less hot. Corticosteroids that are applied to the skin in the form of creams, ointments, lotions, mousses, shampoos, gels or tapes are known as topical corticosteroids (TCSs).
TCSs are available in four different strengths or potencies: mild, moderate, strong and very strong. Your doctor will decide on the correct strength for you based on the nature of your condition, your age, and the area of your body needing treatment.
What skin conditions are treated with topical corticosteroids?
TCS are used to treat a wide variety of inflammatory skin conditions including eczema, psoriasis, allergies, dermatitis, excessive scar tissue and many more.
Will topical corticosteroids cure my skin condition?
The aim of TCS treatment is to control the skin condition rather than cure it.
How should I apply topical corticosteroids?
You should use TCSs as instructed by your healthcare professional, who will explain where, how frequently and for how long you should apply the medication. It is important not to under-use or over-use TCSs.
Usually, you will be told to use enough of the preparation to cover the area to be treated (see information on fingertip units at the end of this paragraph). Apply in the direction of hair growth to minimize the build-up of TCS at the base of hairs as this can cause inflammation of the hair follicles (folliculitis). For instance, on the arm, this means from the elbow towards the wrist.
Your healthcare professional may prescribe more than one TCS, of different strengths, for you to apply to different areas of the body. Some places, for example the face (especially the eyelids), the groin and under the arms or breasts are more prone to side effects than others.
If you are uncertain how to use the TCS, be sure to ask your healthcare professional for clarification.
You may find it useful to complete the section at the end of this information leaflet to remember how frequently you should use the treatment and for how long. Most people who are prescribed topical corticosteroids will also be prescribed an emollient (moisturiser). You can use both treatments at the same time of day but should wait twenty to thirty minutes between the two treatments to avoid diluting the topical steroid which will reduce the effectiveness.
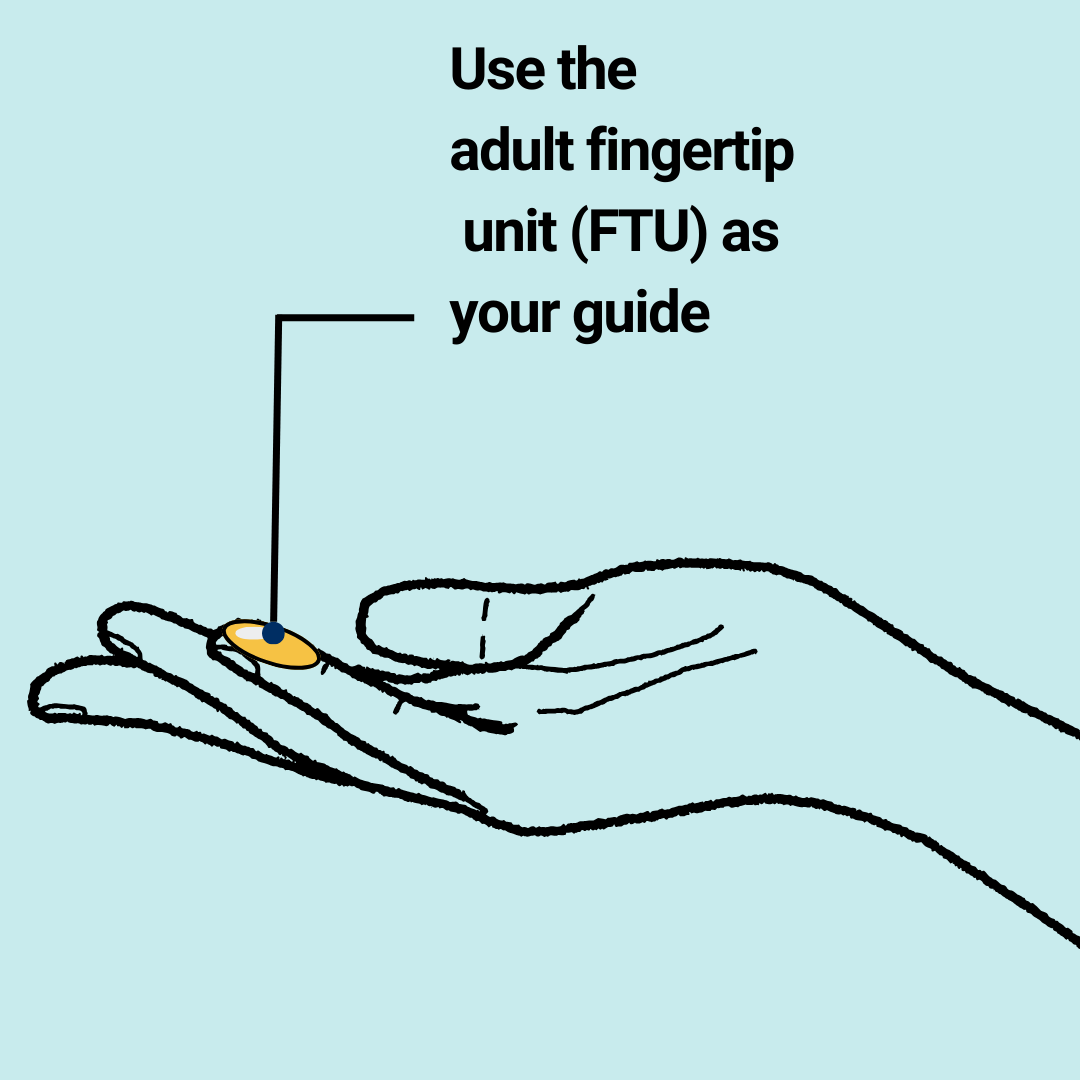
Fingertip Unit Application
A fingertip unit (FTU) is the amount of cream or ointment that just covers the end of an adult finger from the tip to the crease of the first joint when squeezed from an ordinary tube. This is enough to cover an area of skin the size of two hands with the fingers together. This helps to ensure you are using the correct amount of TCS – not too much and not too little.
What are the side effects of topical corticosteroids?
When used as directed by your healthcare professional, the chance of side effects is much smaller and the risk of any absorption of steroids into your blood through your skin is very low. During the first few days of treatment it is common to experience burning or stinging sensations; however this usually goes away after a while.
It is acceptable to use TCS for long periods of time, if advised by your healthcare professional. It is important to know what strength to apply to each affected area of the body, how much, how often, and for how long. However, if TCS (particularly the potent and super-potent ones) are used for a long time, they may cause changes to the treated skin, such as thinning, fragility, bruising more easily, stretch marks, folliculitis and pimples, loss of skin pigment, and hair growth at the area of application. Using less TCS than advised, or stopping the treatment too soon, can make your skin condition difficult to control and may mean that a stronger preparation will be needed to bring your condition under control again.
Occasionally, an allergy to the TCS or to one of the other ingredients of the topical preparation may develop and cause more inflammation.
Is there anything I should do or avoid whilst applying topical corticosteroids?
If a TCS has been prescribed to treat an inflammatory skin condition such as eczema or psoriasis, it is beneficial to also use emollients generously and frequently to help the skin get better.
| CAUTION:
This leaflet mentions ‘emollients’ (moisturisers). Emollients, creams, lotions and ointments contain oils. When emollient products get in contact with dressings, clothing, bed linen or hair, there is a danger that they could catch fire more easily. There is still a risk if the emollient products have dried. People using skincare or haircare products should be very careful near naked flames or lit cigarettes. Wash clothing daily and bedlinen frequently, if they are in contact with emollients. This may not remove the risk completely, even at high temperatures. Caution is still needed. More information may be obtained at https://www.gov.uk/guidance/safe-use-of-emollient-skin-creams-to-treat-dry-skin-conditions.
|
Be sure not to exceed the length of the course of treatment recommended by your healthcare professional.
When should you not apply corticosteroids?
TCSs should generally not be used on broken skin or infections such as impetigo, cold sores and fungal infections (on skin or nails) unless combined with an appropriate anti-infective agent, or advised by your healthcare professional. TCS may worsen some non-infectious skin diseases such as acne, rosacea or peri-oral dermatitis.
TCSs are safe to use in pregnancy and breast feeding, and there is no age limit for their use.
Where can I get more information about topical corticosteroids?
This information sheet does not list all the side effects that this medication can cause. If you would like any further information about topical corticosteroids, or if you have any concerns about your treatment, you should discuss this with your doctor or pharmacist. For full details, please see the drug information leaflet that comes with your medicine.
Web links to other relevant sources:
http://www.eczema.org/corticosteroids
https://patient.info/doctor/topical-steroids-for-the-skin
http://dermnetnz.org/treatments/topical-steroids.html
Jargon Buster: https://www.skinhealthinfo.org.uk/support-resources/jargon-buster/
Please note that the British Association of Dermatologists (BAD) provides web links to additional resources to help people access a range of information about their treatment or skin condition. The views expressed in these external resources may not be shared by the BAD or its members. The BAD has no control of and does not endorse the content of external links.
This leaflet aims to provide accurate information about the subject and is a consensus of the views held by representatives of the British Association of Dermatologists: individual patient circumstances may differ, which might alter both the advice and course of therapy given to you by your doctor.
This leaflet has been assessed for readability by the British Association of Dermatologists’ Patient Information Lay Review Panel
BRITISH ASSOCIATION OF DERMATOLOGISTS PATIENT INFORMATION LEAFLET
PRODUCED | MARCH 2012
UPDATED | MARCH 2015, MAY 2019, JANUARY 2024
NEXT REVIEW DATE | JANUARY 2024
Download a PDF of this page using the link below:
Download File