
What are the aims of this leaflet?
This leaflet has been written to help you understand more about Mohs micrographic surgery (often shortened to Mohs surgery). It aims to explain what this procedure is, what it involves and its potential benefits and risks.
This leaflet also aims to help you decide if Mohs surgery is right for you (alternative treatments include no treatment, traditional surgical skin cancer removal and non-surgical treatments including radiotherapy). You will also find useful information about preparing for Mohs surgery.
What is Mohs surgery?
Mohs surgery is a special type of skin surgery used to remove skin cancers, most commonly basal cell carcinomas. It is named after the surgeon, Dr Frederic Mohs, who developed the technique in the 1930s.
The procedure involves carefully checking the edges of the excised specimen, so the skin cancer can be removed with as much certainty as possible to maximise the chance of clearance.

1. In Mohs surgery, your skin cancer and some surrounding normal-looking skin are removed (stage 1). 2. In the lab, your surgeon will look at the removed specimen to check for cancer cells and to judge if the margins are clear.
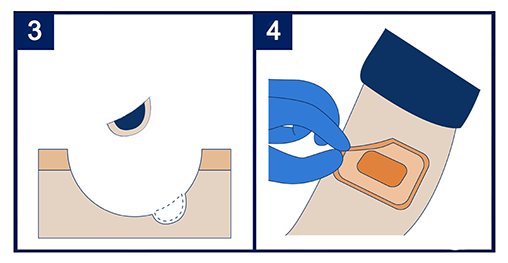
3. Any cancer left behind is removed in the next stage of surgery (stage 2). 4. At the end of the surgery, you are left with a healthy wound which is covered with a dressing.
In 90% of cases the skin cancer is removed after 1-2 stages of Mohs surgery. Some people may need more stages.
Who performs Mohs surgery?
Normally, it is a dermatologist with specialist training in Mohs surgery. If needed, other doctors can repair your wound (for example, maxillo-facial, oculoplastic or plastic surgeons).
When is Mohs surgery used?
Mohs surgery is most often used to treat basal cell carcinomas (BCC) and, in some cases, of squamous cell carcinomas (SCC) and several other rare skin cancers. These skin cancers usually appear on the head and neck region. You may be recommended Mohs surgery if:
- It is difficult to see the edges of the skin cancer and so there would be a chance of not removing it fully if a standard surgical removal was performed.
- You have a skin cancer in an area where it is important to try and preserve unaffected skin and deeper tissue, if possible (for example, on eyelids, nose, ears, lips and around the mouth).
- You have a large skin cancer.
- Your last surgery has not removed all of the skin cancer.
- You have a skin cancer that returned after having surgery.
What are the complications of Mohs surgery?
More common risks:
- Bleeding and bruising – It is normal for the site to bleed during and after your surgery for a few days – usually this is minimal. This is more likely if you take blood thinning tablets or have a condition that causes you to bleed or bruise more easily.
- Pain – you might feel some pain after the surgery. This can be managed with rest and painkillers that can be bought without a prescription (for example, paracetamol).
- Scarring – all skin surgeries will leave a scar.
Less common risks:
- Infection – If your doctor thinks that you have an infection or are at high risk of getting an infection, they may give you some antibiotics.
- Nerve damage – Nerves in the skin can be damaged during the surgery. This can cause the area to feel numb. In rare cases, nerve damage can cause muscle weakness.
- Cancer recurrence – In very rare cases, a skin cancer can return.
How does Mohs surgery compare to standard excision?
Both Mohs surgery and standard excision remove your skin cancer and some surrounding skin. However, there are some differences between them:
Benefits of Mohs
- Mohs surgery is more likely to remove all of the skin cancer in one day. This is because the edges of the skin cancer removed are checked under the microscope on the same day. If any cancer remains, additional surgery can be done on the same day. This is important for skin cancers that can come back or may not be fully removed by standard excision.
- Less healthy skin and deeper tissue may be removed which in some cases may be beneficial and result in a different reconstruction compared to a standard surgical excision
Drawbacks of Mohs
- There are usually longer waiting lists for Mohs surgery compared to standard excision. This is because fewer cases can be completed in the same day. This means your skin cancer could grow while waiting to have Mohs surgery.
- Mohs surgery takes longer to do (half a day on average) than standard excision. More than one set of local anaesthetic injections are often needed for Mohs. It can be a long and tiring day.
- Not all skin cancers should be removed using Mohs surgery. Many skin cancers can be removed easily with standard excision and have good outcomes. Your healthcare professional will discuss this with you based on your circumstances.
What happens before my surgery?
You may be offered an appointment with your dermatologist before the surgery. This is a chance to discuss:
- Your overall health
- Your medications
- The procedure and what to expect on the day that you attend for Mohs surgery
- Any worries you may have
- Aftercare you will need
- Your other options
What happens on the day of my surgery?
You will check in for your surgery at the dermatology department reception as you would for any other appointment. You will usually be taken to a surgical theatre or suite and given a gown to wear.
Your surgeon will examine your skin cancer and use a marker pen to draw around it. They may also take a photograph of your skin cancer. This can help guide your surgeon and will be added to your confidential medical records. Photographs will be shared with and shown toothers only with your written permission.
You will receive an injection of local anaesthetic into the skin to numb the area. This may sting initially, however, will settle within 30 seconds or less.
The surgeon begins by cutting around and under the skin cancer to try and remove all of it the first time. Any bleeding may be stopped with a cautery machine, pressure, or by tying vessels off with stitches. A dressing will be placed on the wound and kept in place with tape. You will then be taken to a recovery bay to wait.
Your skin sample is studied in the laboratory by looking down a microscope while you wait. You will be told if it has been completely removed, or if your surgeon needs to remove more skin or deeper tissue.
How long does Mohs surgery take?
It can take up to 3 hours to get your result. You may need another stage of surgery if any skin cancer was left behind. This means that you could be in hospital for up to a day, although this can vary.
Will I be awake during the surgery?
You will be awake for the surgery, but you will be given an injection of local anaesthetic. This numbs the area but does not send you to sleep. If you need another stage of surgery, you may be given more local anaesthetic.
Some patients ask for some light sedation if they feel nervous during procedures; however, you must discuss this with your surgeon at your pre-assessment appointment. Do not take any such tablets until your surgeon instructs you to, before your procedure.
How will my wound be closed?
Once your surgeon is happy that the skin cancer has been removed, they will discuss with you the options to deal with your wound. There are 5 main ways of dealing with your wound:
- Heal on its own - Your wound will be covered by a dressing and allowed to heal naturally over several weeks / up to 2 months.
- Stitches - The sides of your wound may be stitched together.
- Skin graft - Skin from another place on your body is removed and stitched over your wound.
- Skin flap - Skin from around your wound or from elsewhere is used to cover and close it.
- Referral - You may be referred to another surgical team to reconstruct your wound.
The way your wound is closed will depend on:
- The location of the cancer
- The size of your wound
- The surgeon’s and your preference
Once your wound is closed, it will be covered with a dressing. You will likely then be able to go home. You may be offered an aftercare appointment to replace your dressing or remove your stitches. Your dermatologist or the dermatology nurses will arrange this for you.
What happens after my surgery?
You will receive advice on how to manage any pain from the surgery.
Pain killers such as paracetamol and rest are helpful for the first week or so, until the area starts to settle and heal.
You will need someone to drive you to and from your surgery. Driving and public transport are not advised after your surgery.
Common questions:
When can I drive again?
It may be sensible to avoid driving for several days after your surgery. This can vary and is a decision you can make with your dermatologist. The most important thing is that you wait until you feel comfortable.
When can I go back to work?
This will depend on your work and your recovery from surgery. Generally, you can return to work as soon as you feel comfortable. After bigger procedures with skin flap or graft repair, a week or two off work may be desirable. This is something you can discuss with your dermatologist and workplace.
When can I have a bath / shower?
It is important to keep your dressings dry. You should wait at least 48 hours after your surgery to have a shower. If you have a bath, try and keep your dressing out of the water. This protects your wound while it heals.
Do I need to stop smoking?
Smoking can delay healing after your surgery. It is a good idea to stop smoking for 2 weeks before and after your surgery.
Who can I talk to if I have any other questions?
What do I need to remember for my surgery?
Things to remember to help you prepare for your surgery:
- Food and drink - You can eat and drink on the day of your surgery unless told not to. You can bring your own or buy some at your hospital.
- Comfortable clothes - You can bring a change of clothes for after your surgery
- Something to do - You may have some free time on the day of your surgery. Some people bring a book or phone to keep busy.
- A list of your medications and allergies - This helps your surgeon prepare you for the surgery. It is particularly helpful if there has been any change to your medications since your pre-assessment appointment.
- Transport to and from your surgery - You are advised not to drive or take public transport after having Mohs surgery.
Weblinks to other relevant sources:
Minimum Standards for Mohs’ Micrographic Surgery Services (British Association of Dermatologists and British Society for Dermatological Surgery) 2020
https://bsds.org.uk/mohs-surgery/mohs-standards-2020/
www.bsds.org.uk/patient-information/patient-support-groups

Jargon Buster: www.skinhealthinfo.org.uk/support-resources/jargon-buster/
This leaflet aims to provide accurate information about the subject and is a consensus of the views held by representatives of the British Association of Dermatologists and the British Society for Dermatological Surgery: individual patient circumstances may differ, which might alter both the advice and course of therapy given to you by your doctor.
This leaflet has been assessed for readability by the British Association of Dermatologists’ Patient Information Lay Review Panel
BRITISH ASSOCIATION OF DERMATOLOGISTS PATIENT INFORMATION LEAFLET
PRODUCED | MARCH 2013
UPDATED | APRIL 2016, APRIL 2021, JUNE 2025
Download a PDF of this page using the link below:
Download File