News
Jul 9, 2020
Living with scleroderma during the time of COVID-19
Can you imagine your body being attacked by its own immune system? Cold, numb and painful fingers? Your skin tightening? Aching joints and swollen fingers? Disabling fatigue? These are the features of the condition systemic sclerosis (also known as scleroderma). Here I explain what it’s like to live with and manage, particularly in the time of Covid-19.
What is systemic sclerosis (scleroderma)?
Systemic sclerosis is an auto-immune condition in which the body’s immune system begins to target its own cells and tissues (we call this autoimmunity). This results in damage to the blood vessels, skin and other organs. Scar tissue forms in the skin and other organs preventing them from functioning normally.
It is pronounced “Skleer-uh-dur-muh” and comes from the Greek; ‘sclero’ for hard, and ‘derma’ for skin. This is the most visible effect of the condition although many doctors prefer the term ‘systemic sclerosis’ which better emphasises the effects the condition can have on the internal organs of the body.
Damage to the internal lining of blood vessels is typically the first sign of the disease, and typically presents with symptoms of Raynaud’s phenomenon in the fingers. Raynaud’s phenomenon is the term we use to describe excessive narrowing of the blood vessels of the fingers (and toes, nose and other extremities) in response to cold exposure, leading to the fingers feeling cold, painful, numb and discoloured. Raynaud’s phenomenon itself is actually quite common (about 1 in 20 people) and most people with these symptoms don’t have systemic sclerosis.
Swelling of the fingers and hardening of the skin can be one of the next symptoms to develop. Tightening of the skin is caused by the production of too much scar tissue, and this can occur in other organs of the body including the heart, lungs and gastrointestinal tract. The scar tissue stops the affected parts of the body from functioning normally.

Who does it affect?
Scleroderma affects 19,000 people in the UK and 2.5 million worldwide. Four times as many women as men are affected. It can affect people of any age including children, but is generally diagnosed aged 25 to 55 years. Many people have a good prognosis – they do not die of the disease and live full and productive lives. For others, it can be life-threatening, particularly if it affects the lungs, heart and kidneys.
What are the symptoms?
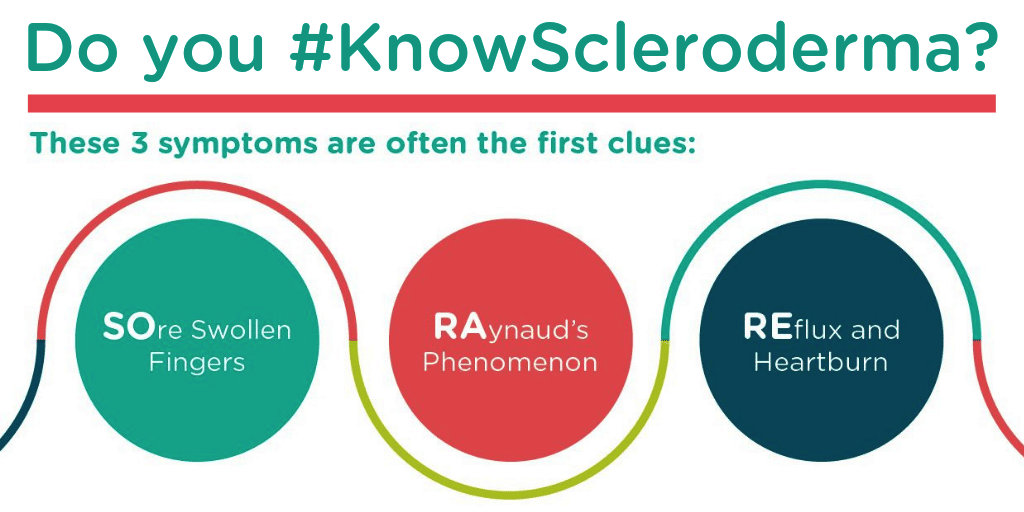
These three symptoms are often the first clues:
SOre swollen fingers or aching joints
RAynaud’s phenomenon – a condition where fingers and toes change colour with temperature changes, stress or anxiety. For 97% of people with scleroderma, Raynaud’s was their first symptom
REflux or heartburn
Types of scleroderma
There are two umbrella types of scleroderma:
- Localised forms are generally limited to different kinds of skin changes and do not have internal organ involvement.
- Systemic forms are complex autoimmune diseases that affect organs throughout the body in addition to skin changes, this can be:
- ‘limited’ refers to the fact that the skin involvement is usually limited to the lower arms and legs, sometimes the face There is still significant internal organ involvement, but it generally develops more slowly than with the diffuse form.
- ‘diffuse’ means people are at greater risk of developing internal organ involvement early in the disease process. The specific internal organ systems that are affected depends to some degree on which specific type of diffuse scleroderma the patient has, often indicated by the patient’s antibody profile.
Living with scleroderma
Cara Hockley, 17, was searching the Scleroderma & Raynaud’s UK (SRUK) website for gloves to help with her Raynaud’s when she realised it might be one sign of a more serious condition. She saw her GP and was diagnosed Dec 2017 with systemic sclerosis. The information from SRUK’s website helped her and her mum get the GP to refer for tests as it’s very rare at her age. It’s steadily got worse for her and now affects her lungs and digestive system. She is very susceptible to infection and has tight skin on her hands and arms – hand sanitiser dries her hands out and hurts her skin ulcers, particularly during the coronavirus pandemic.
Whilst there’s currently no cure, scleroderma can be treated and managed well, meaning that you can continue to live as normally as possible. Treatments and how you manage your condition will vary depending on the type of scleroderma that you are diagnosed with, your symptoms and the ways that these impact upon your life. Looking after your mental and emotional wellbeing can also have a huge impact on the quality of your life.
Particularly, during Covid-19, there are additional challenges facing those with scleroderma. Dr CH Orteu BSc MD FRCP, Consultant Dermatologist, said:
“Frequent and effective hand washing is hugely important in the fight against covid-19 infection, but can also cause irritation and hand dermatitis.
“It is thought that moisturising (emollient) hand washes are not effective at deactivating coronavirus. The current recommendations are therefore to wash hands thoroughly for 20 seconds with soap, pat the skin dry and then apply liberal amounts of your preferred moisturiser.
“If your hands are sore, make sure that you wear gloves for washing up and cleaning, and use lots of moisturiser throughout the day at home. Hand sanitisers should be reserved for use in situations when you are not able to wash hands with soap and water.”
Treating scleroderma
- Look after your skin – use aqueous cream instead of soap, oil-based ointments have longer-lasting effects than water-based creams
- Protect your joints – physios and OTs can help you to manage pain, improve your strength and mobility and how to adapt activities to carry out everyday tasks
- Keep Raynaud’s symptoms under control, for further information visit the SRUK website here
- Take action to prevent and treat ulcers. Cover broken skin with plasters and keep warm
- Keep eyes and mouth from becoming dry. Humidify rooms and steer clear of dry atmospheres. Take sips of water.
- Take care of your gut and bowels. Get enough fluids and eat a healthy balanced diet
- Listen to your body especially if you suffer from fatigue or anxiety – relaxation techniques, mindfulness and regular exercise may help with your mental and emotional wellbeing
- Keep medical appointments – although it was appropriate to reduce non-essential visits to hospital when the pandemic was justifiably the main NHS focus it is important now to seek appropriate advice and have necessary tests to allow diagnosis of complications so that they can be addressed.
Further information on treatments can be found on the SRUK website
Scleroderma & Raynaud’s UK (SRUK) is the only UK Charity dedicated to improving the lives of people with scleroderma and Raynaud’s phenomenon.

This article was written by Dr John Pauling, Consultant Rheumatologist & Senior lecturer
Clinical & Academic Lead for Scleroderma Programme, Royal National Hospital for Rheumatic Diseases (part of Royal United Hospitals Bath NHS FT)