
What are the aims of this leaflet?
This leaflet provides some general information on melanoma skin cancer and the melanoma staging system. In particular, it tells you what stage 3 melanoma is and what will be the investigations/treatments. Details on where to find out more information are also provided at the end of the leaflet.
What is melanoma?
Melanoma is a type of skin cancer, which arises from the pigment cells (melanocytes) in the skin. One of the most important causes of melanoma is exposure to too much ultraviolet light in sunlight. The use of artificial sources of ultraviolet light, such as sunbeds, also increases the risk of getting a melanoma.
Melanocytes make a brown/black pigment (known as melanin), and often the first sign of a melanoma developing is a previous mole changing in colour or a new brown/black lesion developing on the skin. Most frequently there is darkening in colour but occasionally there is loss of pigmentation with pale areas or red areas developing. Occasionally melanomas have no pigment and appear just a pink/red colour. The development of this melanoma on the skin is known as the primary melanoma.
Melanoma is considered to be the most serious type of skin cancer because it is more likely to spread (metastasise) from the skin to other parts of the body than other types of skin cancer. If melanoma has spread to other parts of the body, those deposits are known as secondary melanoma (secondaries/metastases).
What is stage 3 melanoma?
Doctors use a staging system for melanoma to indicate both the likely outcome and the best treatment. The AJCC (American Joint Committee on Cancer) system is currently used in the UK to stage melanoma from 1 to 4. Stage 1 is the earliest melanoma and stage 4 is the most advanced.
The staging system takes into account the thickness of melanoma and if there has been any spread of melanoma from the skin to other parts of the body. Stage 1 and 2 melanomas are present in the skin only and have not spread elsewhere in the body. Stage 3 melanomas have generally spread towards or have reached the draining lymph glands (nodes). Stage 4 melanomas are those that have spread beyond the closest draining lymph glands to other parts of the body.
Lymph nodes, or lymph glands, are found in our lymphatic system, which is part of the body’s immune system. The lymphatics are tiny channels in the skin, which move lymph fluid around the body to the lymph nodes in the groin, under the arms (arm pits) and in the neck. The immune system may fail to destroy the melanoma cells and the cells can then grow within the lymph nodes. If secondary melanoma appears as a lump that can be felt (often about the size of an olive), then you will be diagnosed with stage 3 melanoma
In some patients, a procedure called a sentinel lymph node biopsy is used to detect small numbers of microscopic cancer cells in the nodes, (which cannot be felt). If you have a positive sentinel node biopsy, you will also be diagnosed as having a stage 3 melanoma.
Stage 3 melanoma may also be diagnosed if there are tiny (microscopic) deposits of melanoma in the skin surrounding the primary melanoma (microsatellites), which cannot be seen with the eye but are found by the pathologist when the primary melanoma is removed from the skin. Sometimes these deposits can be seen in the skin near the primary melanoma and they are called in-transit secondaries or satellites. These deposits are considered to be ‘in-transit’ between the primary melanoma and the local lymph nodes. These deposits can be skin coloured or black/blue. They can sometimes be felt just under the skin and are sometimes associated with bruising.
Occasionally a primary melanoma is detected purely as a result of someone developing enlarged lymph nodes with no history of a skin lesion (an occult primary).
Stage 3 melanoma can be divided up into stage 3a, 3b, 3c and 3d. If you wish to know the details about your specific melanoma stage then you can discuss this with a member of your own hospital melanoma team.
Having a stage 3 melanoma means a greater chance that the cancer will come back later somewhere else in the body (stage 4 melanoma). However, this is by no means inevitable. So, developing stage 3 melanoma is a cause for concern but it is still potentially curable.
What tests may be performed when stage 3 melanoma is suspected?
Fine needle biopsy
This is one of the most common tests, and it sometimes termed a fine needle aspiration (FNA). A sample is taken from a suspicious lump using a small needle. The pathologist then examines the sample under the microscope to look for melanoma cells. This test is similar to a regular blood test and typically takes place in the clinic. When the lump is deeper in the tissues, a radiologist (the X-ray doctor) will use a scan to determine where to place the needle. This can be an ultrasound scan or a CT (computerised tomography) scan.
Scans
Scans such as ultrasound, CT (computerised tomography), MRI (magnetic resonance imaging), PET (positron emission tomography) are usually done to check for any further spread of the melanoma in the body. Your melanoma team will explain why they have chosen a particular type of scan - each type has particular advantages. Further details on what these scans may involve can be found on the links provided at the end of the leaflet.
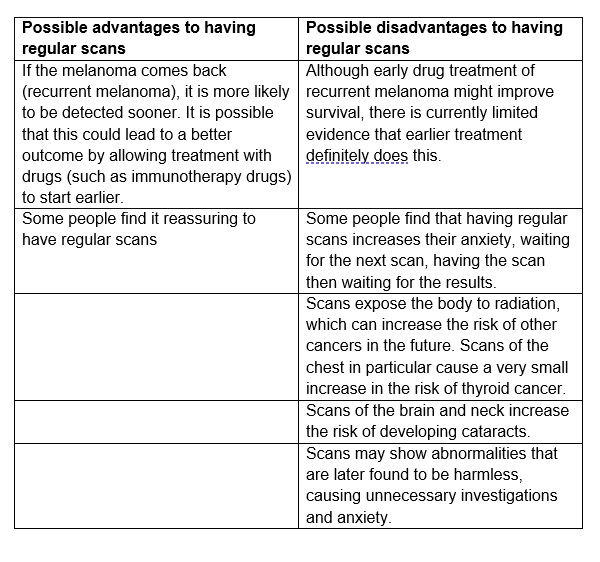
Routine scans can be considered for patients with stage 3 melanoma but the following advantages and disadvantages should be considered.
Possible advantages and disadvantages of having regular scans
Genetic testing on your melanoma
A sample of your melanoma tumour may be sent for genetic testing, in particular to look for a specific gene mutation (a change in the arrangement of the building blocks of your melanoma), known as a BRAF mutation. This gene mutation makes an altered BRAF protein, which makes the melanoma cells grow. Around 50% of melanomas will have a BRAF mutation. If you have changes in the BRAF gene, your melanoma is described as BRAF positive or mutant. If you don’t have changes, then your melanoma is BRAF negative or wild type. Although this information may not be used straightaway, it will help plan any future treatment with drug therapies if needed.
What is the treatment for stage 3 melanoma?
A multidisciplinary team (MDT) of experts will meet to discuss the best treatment option(s) for you. The MDT is made up of dermatologists, surgeons, pathologists, oncologists and specialist nurses A member of the MDT will explain your treatment options to you and you may also meet a melanoma/skin cancer clinical nurse specialist (CNS) who would be a point of contact for you and advise you accordingly.
Treatment options may include some of the following:
1. Surgery
In-transit secondaries
Surgery can be used to remove the in-transit or satellite lumps of melanoma in the skin near your primary melanoma scar, usually under a local anaesthetic (via an injection to numb the skin). This might not be possible when there are many deposits and so other treatments may be discussed with you, such as cryotherapy treatment, isolated limb infusion, or isolated limb perfusion, topical treatment with imiquimod or electro-chemotherapy (ECT).
Lymph node secondaries
If you have spread of melanoma to your lymph nodes which can be felt, then all the lymph nodes in that area are typically removed (lymphadenectomy or complete lymph node dissection) for local control of the melanoma. The aim of the surgery is to remove the cancer to reduce the chance of it recurring in the same place. This is to avoid the melanoma from further growing in this site which may cause pain and lead to skin breakdown.
This surgery takes place while you are under a general anaesthetic (you are put to sleep) and will involve a stay in hospital. Usually during the surgery, drains (plastic tubes) are put in place with one end of the drain in the wound under the skin and the other end attached to a plastic bag. These tubes drain away any blood or lymph fluid from inside the wound and will be removed usually around 2 weeks after the operation.
Following surgery, there is sometimes a fluid collection under the wound known as a seroma, which usually resolves over time. However, one of the possible permanent side effects of a complete lymph node dissection is swelling of the limb known as lymphoedema. This can be mild but may be more troublesome especially in the leg after surgery to the groin, but even then, is usually manageable with the use of compression bandaging/stockings. Other complications of a complete lymph node dissection include scarring, infection, numbness, blood clots particularly if the groin nodes have been removed and stiffness. You will have physiotherapy to help you regain movement. It will help your recovery if you persevere with this.
If you have been found to have stage 3 melanoma following a positive sentinel node biopsy, in the past patients would also have been offered a complete lymph node dissection. However new evidence suggests that this further procedure does not improve survival from melanoma. This is therefore no longer routinely recommended after a positive sentinel node biopsy result.
2. Talimogene laherparepvec (T-VEC)
Talimogene laherparepvec (or T-VEC) is a genetically modified virus that is designed to infect and kill melanoma cells. It has to be injected directly into tumours, so is only suitable for people who have lumps that can be felt (e.g. skin lumps or lymph nodes) with no disease in internal organs, and it is considered when surgery is not an option. Ultrasound guidance may be needed to make the injection safer. Side-effects of T-VEC include pain at the injection site and rashes. You should keep the injection site covered for 48 hours after treatment, and discard dressings in the bin provided by the hospital.
3. Adjuvant treatments/Clinical trials
Adjuvant therapy refers to any additional treatment that is given after a cancer is surgically removed and when there is no other disease visible clinically or on radiological scans. The aim of adjuvant treatments is to stop or slow the growth of any potentially remaining cancer cells (reducing the risk of secondaries). This treatment with be discussed with you by your doctor and may be either treatment with a) targeted therapy or b) immunotherapy.
a) Targeted Therapy
If your melanoma is shown to have a BRAF mutation when it is sent for genetic testing, then targeted therapy with a BRAF inhibitor drug will be suitable for you and works by inhibiting the growth of any melanoma cells which may be present in the body. These are tablets or capsules which are taken twice a day. BRAF inhibitor drugs do not work unless you have a BRAF mutation. A BRAF inhibitor (e.g. dabrafenib) is usually given in combination with a MEK (another building block) inhibitor drug (e.g. trametinib). Side effects of these drugs include rashes, joint pain, high temperature (fever), ECG changes, high blood pressure, changes in eyesight, and weakness of the heart muscle. The adjuvant treatment is for 1 year.
b) Immunotherapy
Immunotherapy is treatment that encourages this action of the body to fight against the melanoma.
Nivolumab and pembrolizumab are drug which targets a protein called a PD1 receptor on the surface of T cells. Blocking of the PD1 receptor activates the T cells to produce an immune response against melanoma cells. It is given as an intravenous infusion every 2 weeks (nivolumab) or every 3 weeks (pembrolizumab). Side effects include tiredness, diarrhoea, feeling sick, skin reactions, changes to liver/kidney function, changes in the function of glands such as the thyroid and adrenals, and eye inflammation. The adjuvant treatment is for 1 year
What is the follow up for patients with stage 3 melanoma?
Patients with stage 3 melanoma will be followed up regularly in the outpatient clinic. In the UK, after a diagnosis of stage 3 melanoma, patients are generally seen about every 3 months for 3 years, then every 6 months to 5 years. At your clinic appointment, you will be examined by either a doctor or a CNS for any further spread of melanoma. It is not unusual for your follow up to be shared between the different doctors, and/or a CNS, involved in your care.
Certainly, it is important to be aware and familiar with your body so that you can recognise a new lump (or lesion) if one appears. If in doubt call your specialist nurse and arrange a sooner appointment with your medical team if concerned.
Self care (What can I do?)
Normally, your CNS will discuss the following with you after treatment:
You can examine your skin
Most people do not develop further melanomas; however, some do and they may also develop other forms of skin cancer. The best way to detect skin cancer is to check all your skin every month (please see Patient Information Leaflet on early detection). Essentially, you are looking for changes in the size, shape or colour of any moles, a new mole, or a mole that looks different to the others. There are patient information web-packages, which outline how to look after your moles (please see the web links at the end of this leaflet).You can also look for recurrence of the melanoma by checking for any new lumps near your primary melanoma scar.
Top sun safety tips:
- Protect your skin with clothing. Make sure you wear a hat that protects your face, neck and ears, and a pair of UV protective sunglasses.
- Make use of shade between 11 am and 3 pm when it’s sunny.
- It is important to avoid sunburn, which is a sign of damage to your skin and increases your risk of developing a skin cancer in the future. However, even a tan is a sign of skin damage and should be avoided.
- Apply a high sun protection factor (SPF) sunscreen of at least 30. However, if you have an organ transplant, it is recommended to use SPF 50, which has both UVB and UVA protection all-year round. Look for the UVA circle logo and choose a sunscreen with 5 UVA stars as well as a high SPF, like this:

- Use this sunscreen every day to all exposed areas of skin, especially your head (including balding scalp and ears) and neck, central chest, backs of hands, forearms and legs, if exposed.
- Apply plenty of sunscreen 15-30 minutes before going out in the sun (ideally, apply it twice) and reapply every two hours when outdoors. You should especially re-apply straight after swimming and towel-drying, even if the sunscreen states it is waterproof.
- Make a habit of sunscreen application, applying sunscreen as part of your morning bathroom routine. If you have an oily complexion, you may prefer an oil-free, alcohol-based or gel sunscreen.
- Keep babies and young children out of direct sunlight.
- The British Association of Dermatologists recommends that you tell your doctor about any changes to a mole or patch of skin. If your GP is concerned about your skin, you should be referred to see a consultant dermatologist or a member of their team at no cost to yourself through the NHS.
- No sunscreen can offer you 100% protection. They should be used to provide additional protection from the sun, not as an alternative to clothing and shade.
- Routine sun protection is rarely necessary in the UK for people with black or dark brown skin tones. However, there are important exceptions to this. For example, sun protection is important if you have a skin condition, such as photosensitivity, vitiligo or lupus, or if you have a high risk of skin cancer, especially if you are taking immunosuppressive treatments (including organ transplant recipients) or if you are genetically pre-disposed to skin cancer. Outside of the UK in places with more extreme climates, you may need to follow our standard sun protection advice.
Vitamin D advice
People who avoid sun exposure may be at risk of low levels of vitamin D. They should think about checking their serum vitamin D levels. If the levels are low, they may consider:
- Taking vitamin D supplements of 10-25 micrograms per day. Your GP can advise on this.
- Consuming more foods rich in vitamin D. This includes oily fish, eggs, meat, butter, fortified margarine and cereals.
Having had a melanoma may impact on future applications for life or health insurance, particularly for the first five years after diagnosis. Equally you may be able to make a claim against any critical illness insurance, you may have taken out prior to the diagnosis of melanoma. If you have particular concerns about this, you should seek financial advice.
Where can I get more advice, support & information about melanoma?
When you have been diagnosed with melanoma you might experience a range of emotions including worry, confusion, or even feeling unable to cope. It will probably help if you discuss and share your thoughts and feelings with someone close. This might be a family member or friend. It could also be your doctor, specialist nurse or another member of the team looking after you.
When you are diagnosed with melanoma, you will be given a lot of information. All this information at once can be hard to take in. If you are not clear about anything during your treatment, please don’t be afraid to ask.
Patient support groups providing information:
Melanoma UK
Melanoma Action and Support Scotland (MASScot)
Web: www.masscot.org.uk
Weblinks to other relevant sources:
British Association of Dermatologists
Skin cancer
Information on sun protection
- Sunscreen factsheet:
skinhealthinfo.org.uk/sun-awareness/the-sunscreen-fact-sheet/ - Sun advice for skin of colour:
skinhealthinfo.org.uk/sun-awareness/sun-advice-for-skin-of-colour/ - Sun protection advice for children and babies:
skinhealthinfo.org.uk/sun-awareness/sun-protection-advice-for-children-and-babies/
Information on vitamin D
www.skinhealthinfo.org.uk/sun-awareness/vitamin-d-information/
Cancer Research UK (CRUK)
- Melanoma skin cancer:
https://www.cancerresearchuk.org/about-cancer/melanoma
- Sun, UV and cancer:
www.cancerresearchuk.org/about-cancer/causes-of-cancer/sun-uv-and-cancer
GenoMEL: The Melanoma Genetics Consortium
- Information on looking after your moles and vitamin D:
genomel.org/info-for-patients/%EF%BF%BCsun-protection-and-vitamin-d-after-a-diagnosis/
Melanoma Focus
- Sentinel Node Biopsy Guideline:
org/news-blog/sentinel-node-biopsy-guideline-publication/
Macmillan Cancer Support
- Melanoma: macmillan.org.uk/Cancerinformation/Cancertypes/Melanoma/Melanoma.aspx
- Information on flaps/grafts: https://www.macmillan.org.uk/information-and-support/soft-tissue-sarcomas/treating/surgery/surgery-explained/skins-grafts.html
- Financial support: http://www.macmillan.org.uk/HowWeCanHelp/FinancialSupport/Financialguidance/Financialguidance.aspx
Lancashire Teaching Hospitals NHS Foundation Trust - The Immunotherapy Video:
https://vimeo.com/252355507/00d629311d
NHS vitamin D advice:
www.nhs.uk/conditions/vitamins-and-minerals/vitamin-d/
Jargon Buster:
https://www.skinhealthinfo.org.uk/support-resources/jargon-buster/
This leaflet aims to provide accurate information about the subject and is a consensus of the views held by representatives of the British Association of Dermatologists: individual patient circumstances may differ, which might alter both the advice and course of therapy given to you by your doctor.
This leaflet has been assessed for readability by the British Association of Dermatologists’ Patient Information Lay Review Panel
BRITISH ASSOCIATION OF DERMATOLOGISTS PATIENT INFORMATION LEAFLET
PRODUCED APRIL 2013
UPDATED FEBRUARY 2019
NEXT REVIEW DATE FEBRUARY 2022
Download a PDF of this page using the link below:
Download File