
What are the aims of this leaflet?
This leaflet has been written to give you information about immunisations (vaccinations), which may be relevant when you are taking medicines that act by suppressing the immune system. This includes information about vaccinations which are:
- Recommended before you start, or while taking, immunosuppressant medicines.
- Safe for you to have while you are taking this treatment.
- Need to be avoided.
Which skin disease treatments can affect the safety of immunisations?
In general, we aim to use treatment in cream or ointment form for skin disease to reduce the need for immune system suppression, but the severity of some conditions means that this is not always possible. Some skin conditions, such as severe eczema, psoriasis and pemphigus, can be difficult to treat fully with creams and ointments, and if this is the case stronger treatments can be given, either orally (taken by mouth) or by injection.
What medicines can suppress the immune system?
Some of the medicines which suppress the immune system are prednisolone, ciclosporin, methotrexate (at higher doses of more than 25 mg per week), mycophenolate mofetil, and azathioprine the treatments known as ‘biological’ agents, for example etanercept, infliximab, adalimumab, rituximab, ustekinumab, secukinumab, brodalumab, guselkumab, ixekizumab, tildrakizumab, certolizumab pegol, risankizumab and bimekizumab. More of these treatments are constantly being developed.
These treatments are often called ‘immunosuppressants’ because they suppress, or reduce, the way the immune system works. In the healthy body, the immune system defends us against infection from bacteria and viruses, but in conditions where the immune system is causing too much inflammation and attacking the body itself, immunosuppressant treatments are used to reduce the activity of the immune system.
Why do I need advice about vaccinations and immune suppression treatment?
Vaccinations (immunisations) are treatments, often given as injections, which prevent or reduce the chances of getting certain infections such as ‘flu, tuberculosis, measles and chickenpox. While taking immunosuppressants individuals may be more susceptible to infection, and it is often recommended that vaccinations against common infections such as ‘flu or pneumococcal infection are given to boost an individual’s defence before or after he or she starts immunosuppressant medicines.
Some vaccinations are ‘live’, meaning that they contain the bacterial/viral infection in a reduced form (called live attenuated) and can cause a mild version of the illness a few days after the vaccination. However, in someone whose immune system is reduced, the live vaccine can cause severe infection; therefore, ‘live vaccines’ may need to be avoided in an individual taking immunosuppressants.
In other vaccinations the bacterium/virus is inactivated/killed, meaning that there is no risk of infection even in a mild form following the vaccination.
General advice
- Ideally, inactivated vaccines should be given at least 2 weeks before treatment but can be given during immunosuppressant treatment.
- Live vaccines, if needed, should be given at least 4 weeks before treatment with immunosuppressants is started.
- Live vaccines should not be given to patients taking high-dose immunosuppressant treatment (see specific advice regarding shingles vaccine here: https://www.nhs.uk/conditions/vaccinations/shingles-vaccination/).
- Live vaccines should not be given within 3 months of stopping prednisolone and other immunosuppressant medicines for at least 12 months after stopping biological treatment.
- Although long-term steroid tablets (or injections of steroid into the muscle) suppress the immune system, steroid creams or steroid joint injections do not. Therefore, it is safe to have live or inactivated vaccinations if you are applying steroids to your skin or having steroid injections into your joints.
- Stopping immunosuppressant medications for the sole purpose of administering vaccines may not be the best course of action, especially when a disease is active. Doctors will discuss (weigh up) the risks and benefits of this with the individual affected.
- Vaccines are not usually triggers for disease flares and they should not be withheld for that reason.
- Additional information on use of specific vaccines is available at:
http://www.patient.co.uk/health/immunisation-1366
What is the advice for the use of live attenuated vaccines in infants born to pregnant women on immunosuppressive therapy or mothers who are breastfeeding whilst on immunosuppressive therapy?
Any infant who has been exposed to immunosuppressive biological treatment from the mother whilst in the uterus during pregnancy, should have any live attenuated vaccination postponed until 6 months of age. In practice, this means that children born to mothers who were on immunosuppressive biological therapy during pregnancy will not be eligible to receive rotavirus vaccine (and will need to defer BCG, if indicated, for 6 months). If there is any doubt as to whether an infant due to receive a live attenuated vaccine may be immunosuppressed due to the mother’s therapy, including exposure through breast-feeding, specialist advice should be sought.
Should I have the influenza vaccination (‘flu jab)?
Ideally, the influenza vaccine (‘flu jab) should be administered before starting the treatment and then further influenza vaccinations should be administered every year while taking the immunosuppressant therapy. This is because the ‘flu jab is safe and effective at reducing the chance of catching ‘flu, which can be a very serious condition, especially when the immune system is not fully active.
The usual vaccine is given as an injection into the muscle of the arm. It contains egg, but other ‘flu vaccines can be egg-free or contain a very low quantity of egg. These may be an option for those who are egg-allergic or those following a vegan diet.
If someone has had a severe reaction (anaphylaxis) to egg products or has an egg allergy with severe/poorly controlled asthma, the vaccine should be given in a specialist centre such as an allergy clinic, if an egg-free vaccine is unavailable.
A nasal influenza vaccine is used for children; as it is a live vaccine it is not suitable for those on immunosuppressant treatment, and as it contains egg, is not suitable for those with severe (anaphylactic) reactions to egg.
The influenza vaccine should be given every year while someone is on immunosuppressant treatment.
Should I have the pneumococcal vaccination?
Pneumococci are bacteria that can cause serious infections such as meningitis or pneumonia. If you are taking immunosuppressant treatment, you are at increased risk of this infection and you should ideally have immunisation with pneumococcal vaccine before you start treatment. You might need a booster immunisation every 5 years.
Pneumococcal vaccine is usually given nowadays as part of the normal childhood vaccine schedule; if this was not completed, then discussion with the GP surgery can establish whether the child of an individual taking immunosuppressant drugs needs a booster.
When should I have pneumococcal/influenza vaccines?
These vaccines should ideally be given at least 2 weeks before the immunosuppressive drug is started.
Do not worry if the immunisations were not given before starting treatment; there are several possible reasons for this:
- The doctor may feel that the treatment should be started without delay.
- It is not always possible for the doctor to be sure in advance that the medicine will be needed long-term, so vaccination may not always be considered necessary.
- The vaccine’s availability may be seasonal, and hence unavailable at the time of starting treatment
If the vaccines were not administered before starting treatment, they can be given by a GP later on the advice of a dermatologist, while already on treatment. Although inactivated vaccines can be given to immunosuppressed patients, the response may be less than in someone not taking such medication. A blood test can be taken to check the response to the vaccine.
Is it important to know whether I have had chickenpox in the past?
Yes. This is because chickenpox can be a serious infection in someone whose immune system is not fully active. Discussion with the doctor/GP can establish whether an individual had chickenpox in the past. A blood test is often requested to check for antibodies to varicella (chickenpox). If an individual is not immune (i.e. no antibodies are detected) vaccination may be offered prior to starting treatment. However, this is not offered via the NHS and must be done privately.
In both adults and children, this involves having two separate injections 4 to 8 weeks apart. As this may delay starting treatment for up to 3 months, the doctor may weigh up the options with the individual.
If there are no protective antibodies in an individual already taking an immune-suppressing medicine, it is important that they inform the doctor/GP about any suspected contact with chickenpox, so they can decide whether an injection of chickenpox antibodies (varicella-zoster immune globulin, VZIG) is needed.
Should I have the shingles vaccine?
There are vaccinations available to prevent shingles. Currently, only people aged 70 to 79 can get vaccinated. However, from September 2023:
- People aged 70-79 will still be able to get vaccinated. They might get one dose of Zostavax (a live vaccine) or two doses of Shingrix (an inactivated vaccine, given 6 to 12 months apart).
- People aged 50 and above, and with a weakened immune system will be offered two doses of the Shingrix vaccine (given 8 weeks to 6 months apart)
- People aged 65-70 will also get two doses of the Shingrix vaccine, 6 to 12 months apart, as they become eligible.
It is considered safe for people on low dose immunosuppressive medication to receive the shingles vaccine. Your doctor will advise if it is safe for you to have this vaccination depending on the dose of your immunosuppressant medicine. Most dermatology patients are on low-dose immunosuppressive medication (see paragraph below).
Are there other infections apart from chickenpox for which I need to watch out?
When on immunosuppressant medicines, if you have been in contact with someone with measles (and you are not immune), you may need an injection of human immunoglobulin.
You are at very slightly increased risk of other infections, caused by bacteria, viruses and fungi. These range from common mild infections such as athlete’s foot and verrucae, to potentially serious ones such as pneumonia and urinary infections. You should see your doctor if you are unwell, or have any persistent symptoms such as fever, cough with phlegm or pain on passing urine.
What should I do if I am planning to travel?
If you are planning to travel while on treatment, then you should let your doctor know. You should avoid live vaccines if you are on high-dose immunosuppressant medication. Your GP surgery may run travel clinics which will be able to provide you with up to date information on which vaccinations are required when travelling to different locations.
Alternatively, a commercial travel clinic, which specialises in immunisations for travellers, will be suitable.
Always inform the doctors and nurses, or those working in the travel clinics, of your medical conditions and the medications you are on.
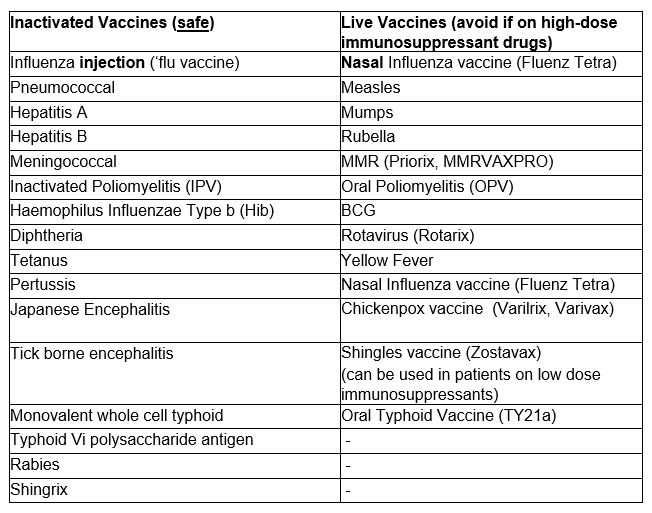
Which vaccines are safe, and which should be avoided when on immune-suppressing medicine?
Which are the patients on ‘high-dose immunosuppressant drugs who must avoid live vaccines?
- Those who are receiving or have received in the past 12 months immunosuppressive biological therapy (for example, rituximab or anti-TNF therapy) should not be given live vaccines.
- If an individual has already been given a live vaccine, then there must be a 4-week interval before the immunosuppressive drug is started.
- If a person has been taking high dose immunosuppressants, then the treatment must have been stopped for at least 3 months before the live vaccine can be given.
High dose immunosuppressants are defined as any of the following:
- Adults and children on prednisolone at the following doses: (greater than 40 mg prednisolone per day or 2 mg/kg/day in children under 20 kg) for more than 1 week
- Adults and children on prednisolone at the following doses: (greater than 20 mg prednisolone per day or 1 mg/kg/day in children under 20 kg) for more than 14 days
- More than 25 mg per week of methotrexate.
- More than 3 mg/kg azathioprine per day.
Below these doses, even if these drugs are used in combination, then live vaccines may be administered.
Vaccines for household members of immunosuppressed people
People who live in a household with immunosuppressed patients should have a ‘flu jab using the inactivated influenza vaccine each year. Other members of the household should be offered MMR and varicella vaccines, if not immune.
Other members of the household should not be given live oral polio vaccination if sharing the same bathroom or toilet. If the live vaccine is given to them, then close personal contact between the immunosuppressed person and the person given the live polio vaccine should be avoided for 4 to 6 weeks. This is because there have been very rare cases of polio infection in contacts of people who have received the live oral polio vaccine.
A safe, inactivated injected polio vaccine (IPV) is now routinely given in the UK for babies having their primary course of immunisations, and this will not cause a problem.
Other live vaccines are safe for household members. For example, live ‘flu vaccine, MMR, rotavirus, shingles and varicella. But if a rash occurs, contact with the affected person should be avoided.
Where can I find out more about immunisation?
https://www.gov.uk/government/collections/immunisation https://phw.nhs.wales/topics/immunisation-and-vaccines/
https://www.gov.uk/government/collections/immunisation-against-infectiousdisease-the-green-book
http://www.patient.co.uk/Search.asp?searchTerm=vaccines&collections=All
Guidance on Covid-19 vaccination:
2013 IDSA guidelines for vaccination:
http://cid.oxfordjournals.org/content/58/3/e44
Jargon Buster: https://www.skinhealthinfo.org.uk/support-resources/jargon-buster/
Please note that the BAD provides web links to additional resources to help people access a range of information about their treatment or skin condition. The views expressed in these external resources may not be shared by the BAD or its members. The BAD has no control of and does not endorse the content of external links.
This leaflet aims to provide accurate information about the subject and is a consensus of the views held by representatives of the British Association of Dermatologists and the United Kingdom Primary Immunodeficiency Network: individual patient circumstances may differ, which might alter both the advice and course of therapy given to you by your doctor.
This leaflet has been assessed for readability by the British Association of
Dermatologists’ Patient Information Lay Review Panel

BRITISH ASSOCIATION OF DERMATOLOGISTS PATIENT INFORMATION LEAFLET
PRODUCED | OCTOBER 2010
UPDATED | DECEMBER 2010, MAY 2015, SEPTEMBER 2022
NEXT REVIEW DATE | SEPTEMBER 2025
Download a PDF of this page using the link below:
Download File